Nursing case studies are detailed analyses of patient cases, exploring symptoms, diagnoses, and care plans. They serve as educational tools, enhancing critical thinking and practical application in nursing practice.
1.1 Definition of a Nursing Case Study
A nursing case study is a detailed analysis of a patient’s health situation, incorporating symptoms, medical history, and assessment findings. It provides a comprehensive overview of the patient’s condition, diagnosis, and treatment plan. This tool aids in understanding the complexities of patient care, facilitating accurate diagnoses, and evaluating outcomes. Nursing case studies are invaluable for education, enabling students and professionals to develop critical thinking and clinical skills through real-life scenarios and evidence-based practices.
1.2 Purpose of Nursing Case Studies
The primary purpose of nursing case studies is to provide a detailed examination of patient care scenarios, enhancing clinical decision-making and critical thinking. They serve as educational tools, allowing nursing students and professionals to analyze real-life situations, identify best practices, and apply evidence-based interventions. Case studies also facilitate professional development by bridging the gap between theory and practice, ultimately improving patient outcomes and advancing nursing knowledge. They are invaluable for training, assessment, and continuous improvement in healthcare settings.
Importance of Nursing Case Studies
Nursing case studies are vital for enhancing clinical skills, promoting evidence-based practice, and fostering professional growth. They provide real-life examples, enriching learning and improving patient care.
2.1 Enhancing Clinical Decision-Making Skills
Nursing case studies provide practical insights into patient care, allowing nurses to analyze clinical data, identify patterns, and refine their decision-making abilities. By examining real-life scenarios, nurses can evaluate symptoms, diagnoses, and interventions, fostering a deeper understanding of evidence-based practices. This process enhances their ability to prioritize care, address complex conditions, and deliver personalized treatment plans effectively. Case studies bridge theory and practice, empowering nurses to make informed, timely decisions that improve patient outcomes.
2.2 Promoting Evidence-Based Practice
Nursing case studies play a pivotal role in advancing evidence-based practice by linking clinical experiences with current research. They provide concrete examples of how evidence informs patient care, allowing nurses to apply proven interventions and outcomes. Analyzing case studies helps identify best practices, evaluate treatment effectiveness, and integrate research findings into daily practice; This fosters a culture of continuous improvement, ensuring that patient care is grounded in the latest scientific knowledge and guidelines, ultimately enhancing patient safety and outcomes.
2.3 Facilitating Student Learning and Professional Development
Case studies are invaluable for nursing students, offering real-life scenarios that bridge theory and practice. They enhance critical thinking, clinical decision-making, and problem-solving skills. By analyzing patient histories, symptoms, and outcomes, students gain practical insights into diverse conditions and care strategies. Case studies also encourage collaboration, as students discuss diagnoses and interventions, fostering a deeper understanding of professional roles and responsibilities, ultimately preparing them for the complexities of clinical practice and lifelong learning in the nursing field.

Structure of a Nursing Case Study
A nursing case study typically includes identifying data, health history, current medications, and assessment findings. These components provide a comprehensive overview of the patient’s condition and treatment plan.
3.1 Identifying Data
Identifying data in a nursing case study includes patient demographics such as age, gender, and medical history. This section provides a snapshot of the patient’s background, including their chief complaint and admission details. It sets the stage for understanding the context of the patient’s condition and subsequent care plan. Accurate and relevant data collection is crucial for developing effective nursing interventions and ensuring comprehensive care. This information guides healthcare providers in delivering personalized treatment.
3.2 Health History
The health history section of a nursing case study details a patient’s past and current medical conditions, surgeries, allergies, and medications. It also includes lifestyle factors such as diet, exercise, and substance use. This comprehensive overview helps identify patterns and risk factors that may influence the patient’s current condition. Accurate documentation of health history is essential for developing a tailored care plan and ensuring continuity of care. It also aids in anticipating potential complications and improving patient outcomes.
3.3 Current Medications
The current medications section lists all prescribed and over-the-counter drugs a patient is taking. This includes dosages, frequencies, and routes of administration. It also notes any supplements or herbal remedies. Documenting medications helps identify potential drug interactions, side effects, and adherence issues. This information is crucial for assessing the patient’s overall condition and tailoring nursing interventions to avoid harm and optimize therapeutic outcomes. Accurate medication records ensure safe and effective care planning.
3.4 Assessment and Findings
The assessment and findings section details the patient’s physical and emotional condition through observation, physical exams, and diagnostic tests. It includes objective data like vital signs, lab results, and imaging, as well as subjective data such as reported symptoms or pain levels. These findings help nurses identify health issues, monitor progress, and inform the nursing care plan. Accurate documentation ensures comprehensive understanding of the patient’s status and guides appropriate interventions. This step is vital for delivering individualized, evidence-based care.

The Process of Writing a Nursing Case Study
Writing a nursing case study involves selecting a patient, gathering data, assessing needs, and developing a care plan. It requires thorough research and analysis to ensure accuracy and relevance, providing a comprehensive overview of the patient’s condition and treatment outcomes. This structured approach helps students and professionals refine their clinical skills and decision-making abilities.
4.1 Selecting a Patient Case
Selecting a patient case involves identifying a scenario that offers valuable learning opportunities. It should be relevant to nursing practice, showcasing unique challenges or common conditions. The case should provide ample data for analysis, including health history, symptoms, and treatment outcomes. Privacy and ethical considerations must be prioritized, ensuring patient confidentiality. The chosen case should align with educational goals, enabling students to apply theoretical knowledge to real-world situations effectively. This step lays the foundation for a comprehensive and meaningful case study.
4.2 Gathering Relevant Data
Gathering relevant data is crucial for a comprehensive case study. This includes collecting the patient’s demographic information, medical history, current medications, and clinical findings. Data should be sourced from medical records, interviews, and observations. Objective data, such as lab results and vital signs, are essential, while subjective data, like patient-reported symptoms, provide additional insights. Ensuring accuracy and thoroughness in data collection is key to forming a complete picture of the patient’s condition and care journey. This step ensures the case study is well-supported and informative.
4.3 Assessing Patient Needs
Assessing patient needs involves identifying physical, emotional, and educational requirements. This step ensures a holistic approach to care, addressing both immediate and long-term needs. Nurses evaluate the patient’s health status, functional abilities, and any gaps in knowledge or support. Tools like NANDA-I taxonomy can guide the identification of specific nursing diagnoses. This assessment lays the foundation for developing targeted interventions and establishing measurable goals for the patient’s care plan, ensuring personalized and effective care delivery.
4.4 Developing a Nursing Care Plan
Developing a nursing care plan involves creating a structured, patient-centered document outlining goals, interventions, and outcomes. It begins with prioritized nursing diagnoses, followed by specific, measurable objectives. Interventions are tailored to address each diagnosis, considering evidence-based practices. The plan is collaborative, involving the patient, family, and healthcare team, ensuring continuity of care. Regular evaluations and modifications are essential to reflect the patient’s progress and evolving needs, ensuring effective and individualized care delivery.

Analysis of Data in Nursing Case Studies
Data analysis in nursing case studies involves interpreting clinical manifestations and assessing human needs to identify patterns and underlying issues, guiding accurate diagnoses and effective care strategies.
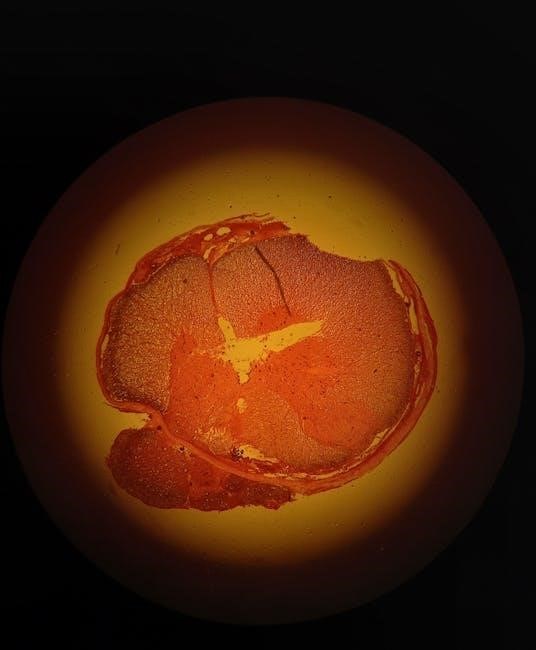
5.1 Clinical Manifestations
Clinical manifestations in nursing case studies refer to observable signs and symptoms presented by patients, such as vital sign abnormalities or physical examination findings. These objective and subjective data are crucial for understanding the patient’s condition, guiding diagnostic processes, and informing care plans. By documenting these manifestations, nurses can identify patterns and deviations from normal, enabling timely and accurate interventions. This step is essential for developing targeted treatment strategies and improving patient outcomes.
5.2 Human Needs Assessment
A human needs assessment in nursing case studies identifies the physical, emotional, and social requirements of patients. This process evaluates factors like pain, mobility, and nutritional needs to create holistic care plans. By addressing these needs, nurses ensure comprehensive and patient-centered interventions. The assessment also considers cultural and psychological factors, promoting individualized care. This step is vital for improving patient outcomes and enhancing the quality of nursing practice.

Nursing Diagnoses in Case Studies
Nursing diagnoses in case studies are identified by analyzing symptoms and related factors, guiding targeted interventions to address patient needs effectively.
6.1 Common Nursing Diagnoses
Common nursing diagnoses include pain, anxiety, and imbalanced nutrition. These diagnoses often stem from clinical manifestations like discomfort, stress, or inadequate dietary intake. Nurses identify these issues through patient assessment and medical history review. For example, a patient with chronic pain may receive a diagnosis of “Acute Pain” related to tissue injury. Addressing these diagnoses ensures personalized care and improves patient outcomes. Each diagnosis guides specific interventions tailored to the patient’s needs.
6.2 Prioritizing Diagnoses
Prioritizing diagnoses involves identifying the most critical issues affecting a patient’s health. Factors like severity, immediacy, and potential impact guide this process. For example, a patient with acute pain and respiratory distress may require prioritizing pain management over nutrition issues. Nurses assess the urgency and patient-centered goals to determine the order of interventions. This ensures timely and effective care, addressing the most pressing needs first to optimize outcomes and patient well-being.
Nursing Care Plan Development
A nursing care plan outlines strategies to address patient needs, focusing on achievable goals. It includes interventions, rationale, and evaluation methods.
7.1 Goals and Outcomes
Goals and outcomes in a nursing care plan are specific, measurable objectives aimed at improving patient health. They are established based on assessments and diagnoses, ensuring a clear direction for care. These goals are patient-centered, addressing physical, emotional, and educational needs. Outcomes are evaluated to determine the effectiveness of interventions, providing a framework for continuous improvement. SMART criteria (Specific, Measurable, Achievable, Relevant, Time-bound) guide the development of these goals, ensuring they are realistic and aligned with patient priorities.
7.2 Interventions and Rationale
Interventions in a nursing care plan are actions taken to achieve desired patient outcomes. These interventions are evidence-based and tailored to address specific needs, such as administering medications, providing education, or implementing lifestyle modifications. The rationale explains the scientific or theoretical basis for each intervention, ensuring they are aligned with best practices and patient-centered care. Documenting interventions and their rationales promotes transparency, accountability, and effective communication among healthcare providers.

Nursing Interventions and Implementation
Nursing interventions are evidence-based actions implemented to address patient needs, such as administering medications or providing education. Effective implementation ensures patient safety and desired health outcomes.
8.1 Non-Pharmacological Interventions
Non-pharmacological interventions are crucial in nursing care, focusing on non-drug approaches to manage patient conditions. These include techniques like deep breathing exercises, positional therapy, and emotional support. For instance, in a pediatric case study, distraction methods such as storytelling or play therapy can reduce anxiety during procedures. Similarly, in geriatric care, establishing a consistent routine helps in managing sleep disorders. These interventions are tailored to individual needs, promoting holistic patient care without reliance on medications. They enhance comfort, reduce stress, and improve overall well-being, making them invaluable in various clinical settings.
8.2 Pharmacological Interventions
Pharmacological interventions involve the administration of medications to treat medical conditions. In nursing case studies, these interventions are carefully documented, including dosage, frequency, and route of administration. For example, in a critical care scenario, antibiotics may be prescribed to treat infections, while pain management often requires analgesics. Nurses must monitor for side effects and ensure adherence to prescribed regimens. Effective pharmacological interventions are tailored to individual patient needs, improving outcomes and supporting recovery. They play a vital role in evidence-based nursing practice, ensuring safe and effective care delivery.

Evaluation of Patient Outcomes
Evaluation of patient outcomes involves assessing the effectiveness of care through measurable goals and documented progress. This ensures quality improvement and informed decision-making in nursing practice.
9.1 Measuring Effectiveness of Care
Measuring effectiveness of care involves assessing whether interventions meet patient goals. This includes monitoring symptom improvement, functional status, and adherence to treatment plans. Tools like assessment scales and lab results help quantify outcomes. Regular evaluation ensures care aligns with evidence-based practices and patient needs, promoting high-quality, patient-centered outcomes. This process guides adjustments to care plans and improves future interventions, ensuring optimal results for patients.
9.2 Documenting Patient Progress
Documenting patient progress involves recording changes in symptoms, functional status, and responses to interventions. Accurate and timely documentation ensures continuity of care and informs future decisions. Notes should include objective data, such as vital signs and lab results, as well as subjective feedback from patients. This documentation also serves as a legal record and communicates patient status to the healthcare team. Regular updates help track progress toward goals and guide adjustments in the care plan.

Examples of Nursing Case Studies
Examples include pediatric, geriatric, and critical care case studies. These real-world scenarios provide practical insights, helping nurses apply theoretical knowledge to diverse patient situations effectively.
10.1 Pediatric Nursing Case Study
A pediatric case study involves a detailed analysis of a child’s health condition, treatment plan, and outcomes. For example, a 10-year-old girl presenting with fever and rash was diagnosed with Kawasaki disease. The study outlines her symptoms, lab results, and nursing interventions, emphasizing family-centered care and education. Such cases highlight the importance of early diagnosis and age-appropriate interventions in pediatric nursing, ensuring holistic care and optimal recovery.
10.2 Geriatric Nursing Case Study
A geriatric case study focuses on the care of elderly patients, addressing age-related health issues. For instance, a 95-year-old male with a history of excellent health experienced sudden decline, requiring hospital admission. The study details his symptoms, medical history, and nursing interventions, emphasizing pain management, nutrition, and mobility. Such cases underscore the need for comprehensive geriatric care, prioritizing comfort and quality of life while managing chronic conditions and promoting patient dignity.
Critical care nursing case studies involve high-acuity patients requiring intensive interventions. For example, a patient admitted with severe respiratory distress received oxygen therapy and blood cultures. The case study outlines the clinical manifestations, such as low oxygen saturation, and the nursing interventions implemented to stabilize the patient. These studies highlight the importance of rapid assessment, evidence-based interventions, and collaborative care in critical settings, ultimately improving patient outcomes and demonstrating advanced nursing skills.
Writing nursing case studies presents challenges like ensuring patient confidentiality and maintaining objectivity. These issues require careful data handling and unbiased analysis to uphold ethical standards. Maintaining patient confidentiality is a critical challenge in writing case studies. Nurses must protect sensitive information by omitting identifiable details, using pseudonyms, and ensuring compliance with HIPAA guidelines. This requires careful redaction of records and strict adherence to ethical standards to safeguard privacy while still providing comprehensive case details for educational purposes. Proper handling of data is essential to prevent breaches and maintain trust in the healthcare system. Maintaining objectivity in case study analysis is crucial for accuracy and reliability. Nurses must avoid personal biases, focusing solely on evidence-based data. This ensures that interpretations remain unbiased and grounded in factual information. By adhering to standardized assessment tools and evidence-based practices, nurses can enhance the credibility of their case studies, providing clear and impartial insights into patient care and outcomes. This approach fosters professionalism and trust in the analysis. Best practices include clarity, conciseness, and evidence-based resources. Use standardized formats, ensure patient confidentiality, and maintain objectivity. Regularly review and update content to reflect current standards. Clarity and conciseness are essential in nursing case study writing. Use straightforward language and avoid overly complex terms. Ensure each section is concise, focusing on key points without unnecessary details. Organize information logically, using clear headings and subheadings. Bullet points or lists can enhance readability. Always prioritize precision to ensure the content is easily understood and applicable to clinical practice. These principles help healthcare professionals quickly grasp and apply the knowledge effectively. Incorporating evidence-based resources is crucial for credibility in nursing case studies. Utilize peer-reviewed journals, clinical guidelines, and reputable textbooks to support your analysis. Properly cite sources to maintain academic integrity and provide a foundation for your conclusions. This ensures that the case study aligns with current best practices and offers actionable insights for patient care. Always reference the most recent and relevant studies to strengthen your nursing interventions and recommendations. Nursing case studies are invaluable educational tools, enhancing critical thinking and evidence-based practice. They provide practical insights, preparing future nurses for real-world challenges and improving patient care outcomes effectively. Nursing case studies are essential educational tools, offering detailed patient histories, diagnoses, and care plans. They enhance critical thinking, clinical decision-making, and evidence-based practice. By analyzing real-world scenarios, nurses develop proficiency in assessing patient needs, prioritizing care, and implementing effective interventions. Case studies also emphasize ethical considerations and interdisciplinary collaboration. They provide valuable insights into diverse specialties, from pediatrics to geriatrics, serving as practical resources for both students and practicing nurses to improve patient outcomes and advance professional development. Nursing case studies are integral to nursing education, bridging the gap between theory and practice. They provide real-life scenarios that enable students to analyze symptoms, diagnoses, and interventions. Case studies foster critical thinking, decision-making, and problem-solving skills. By examining patient histories and care plans, students gain practical insights into diverse clinical situations. This experiential learning enhances their ability to apply evidence-based practices and develop compassionate, patient-centered care. Case studies are invaluable for preparing future nurses to navigate complex healthcare challenges effectively.10.3 Critical Care Nursing Case Study
Common Challenges in Writing Nursing Case Studies
11.1 Ensuring Patient Confidentiality
11.2 Maintaining Objectivity in Analysis
Best Practices for Nursing Case Study Writing
12.1 Clarity and Conciseness
12.2 Use of Evidence-Based Resources
13.1 Summary of Key Points
13.2 The Role of Case Studies in Nursing Education

